Join the Self-Insured Employer Bill of Rights Petition
It’s estimated by experts that $1 out of every $3 spent on healthcare is wasted. Per the 2017 report by the Commonwealth Fund, the United States spends nearly twice as much per capita on healthcare than other high-income countries in the world, with healthcare spending representing over 14% of gross domestic product. These costs are forecasted to continue to grow at 6% per year for the foreseeable future (nearly three times the rate of inflation).
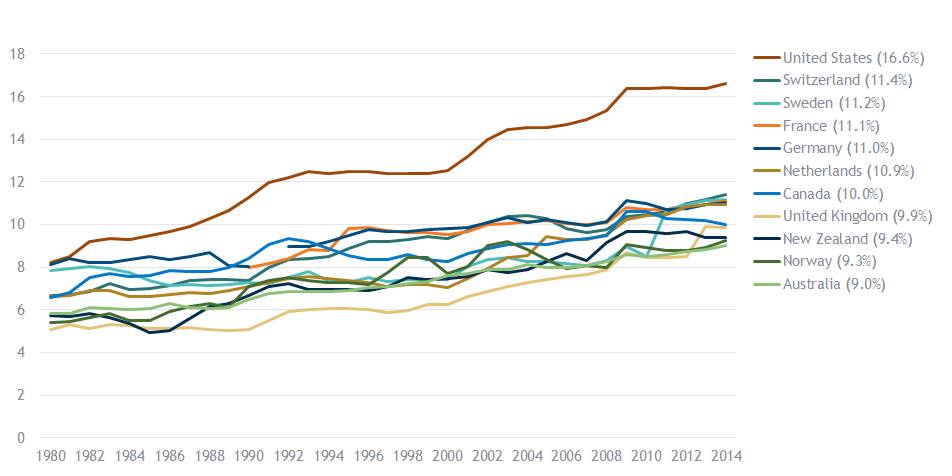
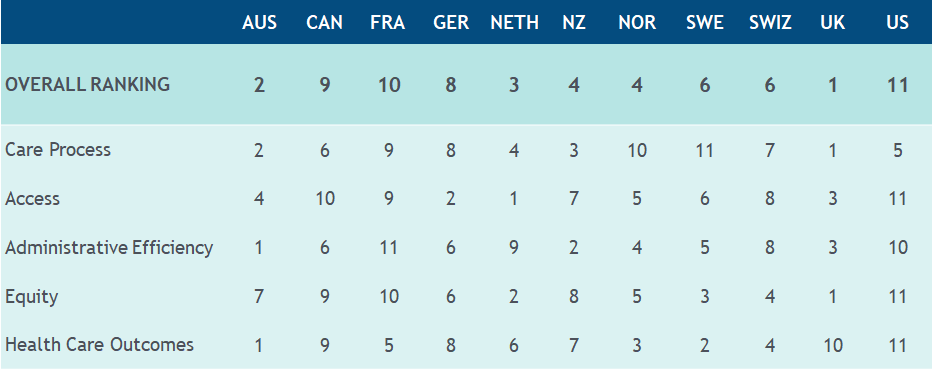
Despite this level of spending, the U.S. ranks dead last among 11 developed economies on the quality of healthcare delivered per the Commonwealth Fund, and has much higher mortality rates than other countries in such areas as respiratory, circulatory, nervous, endocrine and behavioral health per the Peterson-Kaiser Health System Tracker.
Ranking of Countries By Healthcare Quality
Contributing to the explosion in healthcare costs are very high error rates in processing medical claims, as well as large variations in the costs of negotiated medical procedures, even within the same geographical area. According to the Centers for Medicare & Medicaid Services, errors such as improper coverage, coding and billing of medical costs in 2017 was 9.5%. There are estimates that another 10% to 40% of the cost of healthcare is for charges up to ten times the fair market value for care.
Healthcare costs are a significant expenditure for self-insured organizations and in fact, represent one of our largest budgeted costs. Additionally, we serve as the health plan sponsor, and owe a duty to our employees and company to ensure we are fulfilling our fiduciary role as a plan sponsor. Therefore, we require timely and detailed access to our healthcare data, claims, and all supporting documentation for those expenditures.
If you’ve never requested access to your own paid healthcare claims data, the concerns expressed below in the “Self-Insured Employer Bill of Rights” may not be immediately apparent. Upon request of your healthcare claims data and supporting claim documentation, the large third-party administrators (TPA) generally provide a level of responsiveness ranging from plodding accommodation (6 months or more) up through outright defiance and refusal. This in addition to the TPA having numerous, often undisclosed ways to profit from their relationship with a self-funded plan over and above “Per Head” fees.
Further, many of us are publicly held companies. Therefore, our TPA must capture & retain sufficient claims & medical documentation to fulfill the requirements of Sarbanes-Oxley. In the event of questions by us or our employees, the records need to be adequate to verify that we were billed accurately, only for eligible employees, spouses and dependents and charged a competitive, market-based fee negotiated in an arms-length transaction by the carrier.
Because of the escalating medical and pharmaceutical costs, the high rate of billing errors, large variations in pricing for the same procedures in the same geographic area and the overall lack of transparency over “our” data, we hereby execute the following “bill of rights”:
Self-Insured Employer Bill of Rights
Ownership of Claims Data
Claims data is owned by us, the self-funded employer. The third-party administrator (TPA) functions as a medical payment processor on our behalf, but is not granted ownership rights over our medical and pharmacy claims data. We expect our TPA to share the price you paid with OUR checkbook to a provider. Unwillingness for us to verify paid amounts versus the contract terms is a violation of Sarbanes-Oxley (controls must be documented, maintained and tested on at least an annual basis).
Timely Access to Our Claims Data
We are the plan sponsor and owe a duty to our employees and our company to ensure we are fulfilling our fiduciary duties. We cannot achieve this if our TPA refuses to send us complete, accurate data on a timely basis.
Broker/Consultant Compensation
We have hired a broker/consultant as our objective subject matter expert to be our primary advisor on healthcare issues. We do not support the payment of undisclosed fees by the third-party administrator directly to the broker/consultant as this compromises their independence as an advisor.
Full Disclosure of All Fees
TPA’s often have undisclosed fees embedded within the self-funded plan. In addition to the more clearly communicated “Per Head” fees, we require full disclosure of any and all fees including but not limited to the following:
- Network access fees
- Out-of-network discount negotiation fees
- Pharmaceutical rebates
- Educational fees
- Subrogation fees
- Claims audits fees
- Pre-certification
- Nurse hotline
- Telehealth services
- Wellness programs administered by carrier affiliates
- Selling of clients’ data to third parties
- Perform 100% electronic testing of claims for various types of errors;
- Select as large a sample as needed to gain comfort over internal controls (not be limited to 250 or less);
- Request additional claims when error rates are at a higher level than our expectations;
- Take as long as needed to perform that audit (versus being limited to a specific number of days);
- Retain a firm on a contingent fee basis to conduct a thorough audit;
- Have full access to the claims data, as well as the supporting medical records as needed to fulfill our obligations under Sarbanes-Oxley;
- Gain unrestricted access to the contracts you have negotiated on our behalf; and,
- Impose financial sanctions on the TPA if they have been negligent in the performance of their fiduciary duties.
Many of these fees are paid to affiliates of the carrier, and do not represent arms-length transactions. We require at a minimum that these fees are to be disclosed on at least a monthly basis to the self-funded employer.
Performance Guarantees
Performance guarantees need to be calculated and verified by a party independent of the carrier in order to be considered objective and without financial bias.
Adequate Claims & Medical Documentation
Our carrier must capture & retain sufficient claims & medical records documentation to fulfill the requirements of Sarbanes-Oxley. We as a public company need to independently verify that our health plan and employee are being billed accurately, only for eligible participants and charged a competitive, market-based fee negotiated in an arm’s length transaction by the carrier. We require immediate access to claims, medical records and provider contracts to gain assurance that we are only paying for necessary medical products & services prior to reimbursing the provider.
Audit Rights
Carrier must provide open and unrestricted access to claims & data to enable comprehensive audits of our own healthcare expenditures. We should have full ability to:





